Spinal Surgery Techniques: What Are Your Options?

When “spinal surgery” is mentioned, the initial reactions often include “fear” and “anxiety” about the possibility of walking again post-surgery, the fear of being bedridden, or facing paralysis for life, among other concerns. It’s understandable to harbor such fears, as these outcomes have indeed occurred in the past.
Rewinding to a time when surgical tools were not as advanced as they are today, treating spinal conditions was a significant undertaking. The absence of X-ray machines, high-magnification surgical cameras, adequate surgical lighting, and a scarcity of surgeons trained in specialized procedures necessitated large incisions based on the number of affected spinal segments. This approach led to numerous complications during and after surgery, such as excessive blood loss leading to fatalities during operations, severe postoperative pain, and various surgical complications. These factors contributed to the apprehension felt by patients and their families regarding spinal disease treatments. However, in recent times, the evolution of spinal surgery technology and techniques has seen remarkable progress. Today’s surgical approaches, which are tailored to target specific lesions, significantly reduce blood loss, muscle damage, and postoperative complications compared to traditional methods. Additionally, the shortened hospital stays enable patients to resume their normal lives much sooner.
Surgical Wound Length and Recovery Time: What to Expect
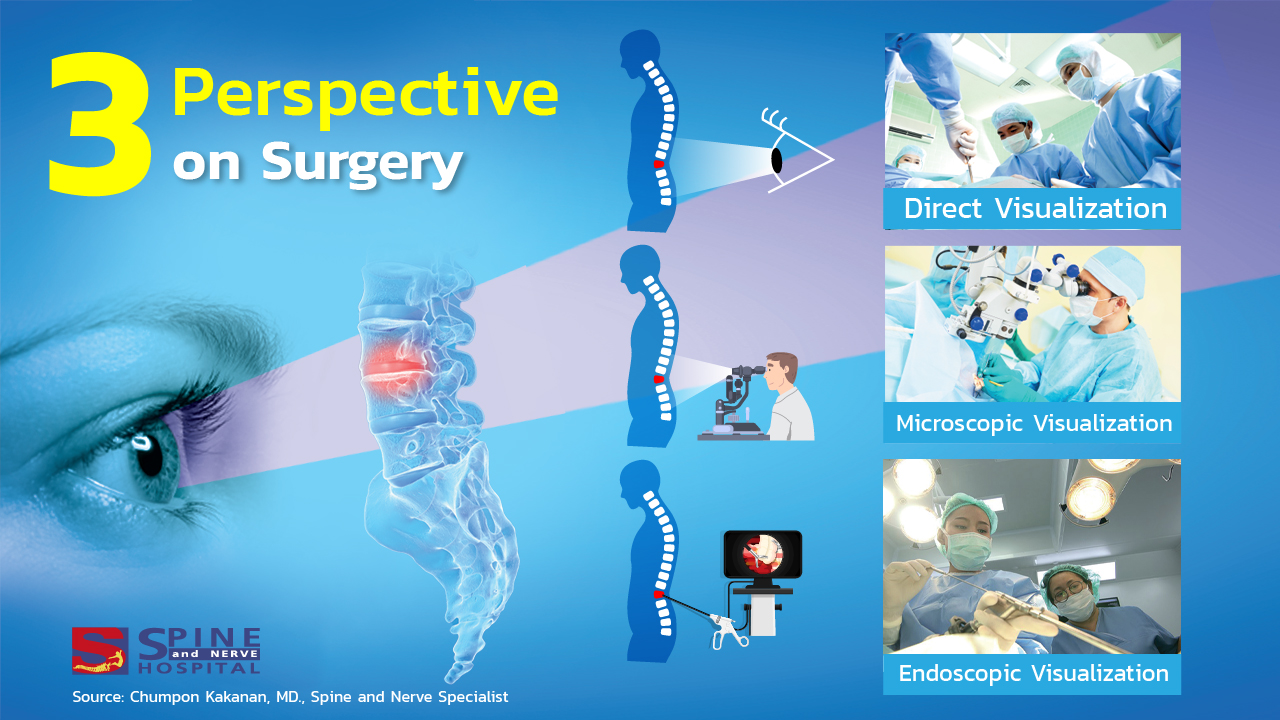
Comparing surgical procedures from the past to the present, it’s evident that operations involving large incisions are based on the number of spinal joints affected. Typically, surgery on a single spinal level results in a wound about 2–7 cm long, while a procedure on two levels might extend the incision to approximately 10–12 cm. Consequently, patients might need a hospital stay of 7–10 days or longer, alongside ongoing physical therapy to avoid muscle atrophy.
The use of high-magnification microscopes have significantly reduced wound sizes to between 3 and 5 centimeters. This improvement not only enhances safety but also shortens the required hospital stay to roughly 3–4 days. However, patients with lower physical strength or the elderly, especially those with pre-existing conditions, must undergo physical therapy to ensure muscles regain their normal function.
Endoscopic spinal surgery, a minimal invasive technique, employs an endoscope’s lens placed at the end of the camera, acting as the surgeon’s eyes inside the patient’s body. This method allows for selective removal of problematic areas without disturbing the surrounding healthy muscle tissue, yielding results comparable to those of major surgery.The key benefit is the minimization of the surgical wound to just 0.5 cm, enabling patients to leave the hospital after just one night and quickly resume their everyday lives without the need for extensive physical therapy.
The array of spinal surgery techniques available today offers various options, with newer technologies generally carrying higher costs. However, these advancements also mean reduced surgical risks and injuries, allowing for a quicker return to daily activities post-surgery.
S Spine and Nerve Hospital, specializing in spine and nervous system treatments, extends its best wishes to all.
Contributor:
Chumpon Kakanan, MD.
Spine and Nerve Specialist